Slade and Royal Arsenal Osteopathic Practice
Covid-19 Policy and Procedure document
Please find below our Covid-19 Policy and Procedure document. You can also download this as a pdf here.
Version 0.9
07.06.2020
| Version | Date | Author | Amendments |
| 0.9 | |||
The Osteopaths: Adapting our practice
Introduction
In the current emergency context of COVID-19, all osteopaths and massage therapists who are practising must ensure that they protect their patients and the public, themselves and others, and should ensure that they have read and implemented as appropriate, relevant and updated guidance to the country in which they are practising. For the purpose of safe practice all patients and practitioners are assumed to be potentially infected and therefore all measures are designed to prevent transmission of infection.
To ensure that we are able to provide osteopathic care whilst also meeting out obligations to public health and protecting our patients, our families, communities and ourselves from infection we have developed this policy and procedure document. It is divided into 7 sections.
The first section details our policy towards practice aligned to the Osteopathic Practice Standards (OPS). Subsequent sections are informed by current guidance from a range of sources, including the General Osteopathic Council[1], The Institute of Osteopathy[2], The National Council for Osteopathic Research[3], Public Health England[4]
Guidance
The Osteopathic Practice Standards provide as follows:
Standard C5 states:
‘You must ensure that your practice is safe, clean and hygienic, and complies with health and safety legislation.’
The associated guidance provides that
- Your practice premises must be clean, safe, hygienic, comfortable and appropriately equipped.
- There are detailed requirements in law for health and safety in the workplace. Further details can be found on the website of the UK Health and Safety Executive.
- You must have adequate public liability insurance.
- You should ensure that you have appropriate procedures in place in the event of a medical emergency.
- You should take all necessary steps to control the spread of communicable diseases.’
Standard D11 states: ‘You must ensure that any problems with your own health do not affect your patients. You must not rely on your own assessment of the risk to patients.
The associated guidance states:
- If you know or suspect that your physical or mental
health is impaired in a way that might affect the care you give to patients, you
must:
- seek and follow appropriate medical advice on whether you should modify your practice and in what way
- if necessary, stop practising until your medical adviser considers you fit to practise again
- inform the GOsC.
- If you are exposed to a serious communicable disease, and you believe that you may be a carrier, you should not practise until you have received appropriate medical advice, and you should follow any advice you are given about suspending or modifying your practice. You should take all necessary precautions to prevent transmission of the condition to patients.
The following guidance addresses these
standards. We will continue to monitor current guidance to ensure that we are
adhering to best practice and responding to changing situations appropriately.
Deciding who can be treated
Triaging
Before any face-to-face appointments can be made it is important that patients are assessed to identify if they have any coronavirus symptoms or they are vulnerable or extremely vulnerable people at significant risk of serious illness. To guide our decision making the following criteria should be applied.
Who is it appropriate to see face-to-face?
Currently England is still in partial lock down. Although restrictions to practice in England have eased in relation to who can be treated, at this time, current guidance is that we should primarily be conducting remote consultations before a face to face appointments to conduct risk assessments and to limit contact time within the practice.
Patient assessment: Standard pre-screening criteria for COVID-19
Patients with coronavirus symptoms should not be attending our clinics. Patients with symptoms of coronavirus should be advised to use the NHS 111 online coronavirus service if they have:
fever ≥37.8°C and at least one of the following which must be of acute onset:
- persistent cough (with or without sputum),
- hoarseness,
- nasal discharge or congestion,
- shortness of breath,
- sore throat,
- wheezing,
- sneezing.
- Direct contact with a known case of COVID-19 within 14 days
The guidance has also recently added the following symptoms
- Acute loss of sense of smell or taste. This is thought to be an early symptom of infection.
Any patients who you suspect of having covid-19 should be advised to contact NHS 111.
Other patients
We must be aware of guidance related to clinically vulnerable and clinically, extremely vulnerable people related to risk.
Clinically vulnerable patients are at higher risk of severe illness from coronavirus. They should take particular care to minimise contact with others outside their household. In England the guidance has stated that clinically vulnerable patients can be treated if in need of urgent care.[5]
Assessment of risk in relation to attending an appointment should be made in discussion with the patient on a case-by-case basis prior to booking a face-to-face appointment. Online consultations should be offered as the first option for care.
Clinically vulnerable people are those who are:
- aged 70 or older (regardless of medical conditions)
- under 70
with an underlying health condition listed below (that is, anyone instructed to
get a flu jab as an adult each year on medical grounds):
- chronic (long-term) mild to moderate respiratory diseases, such as asthma, chronic obstructive pulmonary disease (COPD), emphysema or bronchitis
- chronic heart disease, such as heart failure
- chronic kidney disease
- chronic liver disease, such as hepatitis
- neurological conditions, such as Parkinson’s disease, motor neurone disease, multiple sclerosis (MS), or cerebral palsy
- diabetes
- a weakened immune system as the result of conditions such as HIV and AIDS, or medicines such as steroid tablets
- being seriously overweight (a body mass index (BMI) of 40 or above) o pregnant women
Clinically extremely vulnerable patients are strongly advised to stay at home at all times and avoid any face- to-face contact if they are clinically extremely vulnerable to protect themselves. All patients should be in possession of a letter confirming their extremely vulnerable status.
This is called ‘shielding’. Shielding means:
- Do not leave their house.
- Do not attend any gatherings. This includes gatherings of friends and families in private spaces, for example, family homes, weddings and religious services.
- Strictly avoid contact with someone who is displaying symptoms of coronavirus (COVID-19), see above.
Clinically extremely vulnerable people may include the following people. Disease severity, history or treatment levels will also affect who is in the group:
- Solid organ transplant recipients.
- People with specific cancers:
- people with cancer who are undergoing active chemotherapy
- people with lung cancer who are undergoing radical radiotherapy
- people with cancers of the blood or bone marrow such as leukaemia, lymphoma or myeloma who are at any stage of treatment
- people having immunotherapy or other continuing antibody treatments for cancer
- people having other targeted cancer treatments which can affect the immune system, such as protein kinase inhibitors or PARP inhibitors
- people who have had bone marrow or stem cell transplants in the last 6 months, or who are still taking immunosuppression drugs
- People with severe respiratory conditions including all cystic fibrosis, severe asthma and severe chronic obstructive pulmonary (COPD).
- People with rare diseases that significantly increase the risk of infections (such as SCID, homozygous sickle cell).
- People on immunosuppression therapies sufficient to significantly increase risk of infection.
- Women who are pregnant with significant heart disease, congenital or acquired.
What does this mean in practice?
Prior to considering any face-to-face appointments we must evaluate the following:
- Has the person experienced any symptoms of coronavirus infection?
- Have they been in contact with any patients suffering with COVID 19 in the past 14 days?
- Are they or are they living with or are they themselves a patient who is either vulnerable or extremely vulnerable and consequently at severe risk of serious illness if they were to contract COVID 19?
Following remote consultation, you should carefully decide if it is appropriate to book a follow-up face-to-face appointment given the potential risks of infection. In this instance we should apply the criteria defined for an initial face-to-face consultation and/or consider if there is a need for medical referral.
If you
book any patients in for a face to face appointment please emphasis that
they should inform us immediately if they develop any of the above symptoms or
just feel unwell. They will receive an email reminder 48 and 24 hours and a
text two hours before their appointment which will prompt them to inform us of
any symptom or illness development. They will not be charged for any cancellations
due to illness.
Online Consultation
For the foreseeable future we will be screening patients / clients via our remote telehealth system for risk assessment and take a full case history to reduce face to face contact time. For those patients deemed inappropriate for face to face appointments The GOsC have provided guidance for the provision of remote consultations.[6] Below are the 10 key principles we are expected to apply:
- Make patient safety the first priority and where appropriate raise concerns if the service or system they are working in does not have adequate patient safeguards including appropriate identity and verification checks.
- Understand how to identify vulnerable patients and take appropriate steps to protect them.
- If unfamiliar with the patient, tell them [your] name, role and professional registration details, establish a dialogue and make sure that all patients understand how the remote consultation is going to work.
- Explain that:
- [you] can only provide advice and guidance if [you] feel that it is safe to do so.
- It’s not safe if [you] don’t have sufficient information about the patient’s health or if remote care is unsuitable to meet their needs.
- It may be unsafe if relevant information is not shared with other healthcare providers involved in their care.
- If in [your] judgement [you] can’t provide advice or guidance to the patient because it’s unsafe to do so, [you] will signpost to other appropriate services.
- Obtain informed consent: ensuring it is provided voluntarily by an appropriately informed person with the capacity to consent to the intervention in question in accordance with the requirements of the Osteopathic Practice Standards in this respect.
- Undertake sufficient assessment to establish a clinical rationale for the provision of advice and any remote intervention, where possible with access to existing records in the case of continuing patients.
- Give patients information about all the options available to them, including declining treatment, in a way they can understand.
- Make appropriate arrangements for follow-up care where indicated. If appropriate, and with the patient’s consent, share information with other health and care providers for the enhancement of their care.
- Keep notes that fully explain and justify the decisions they make.
- Stay up to date with relevant training, support and guidance for providing healthcare in a remote context.
Further
guidance has been provided by the iO[7].
In summary these types of consultation are not intended to replace the face to
face/hands on care that is fundamental to osteopathic practice and will not be
suitable for all cases. They should be considered and conducted in the same
manner as you would conduct your in-clinic consultations.
Taking precautions in practice
Before any consultations occur, it is critical that we ensure that the clinical environment is safe. We have taken steps to adapt our clinics to enable us to maintain high standards of clinical hygiene that is easy to disinfect whilst maintaining an appropriate environment for patient care and maintaining social distancing. However, we also need to follow careful cleaning and hygiene procedures before and after an appointment to minimise any risk of transmission of the virus. The following procedures should be adhered to at all times when preparing the clinic to receive a patient.
Cleaning and hygiene
- Practitioners should ensure that the treatment room is aerated for at least 15 minutes between patients (without anyone present). This can be done by either opening the window/door to enable full aeration. Alternatively, an air filtration system with the ability to remove particles less than 0.015 microns may be used.
- All surfaces and equipment in the consultation room and waiting room (if in use), door handles, treatment table (with special attention to the face hole if used) should be cleaned with appropriate detergent. Close attention should be given to surfaces that patients routinely come into contact with. PPE should be worn throughout the cleaning process
- Hand washing/sanitising routines should be followed before, during and after each appointment as appropriate. Any hand sanitiser used should be 60% alcohol based and once fully applied should be allowed to dry for 30 seconds to ensure hands are safely disinfected.
- We will provide hand sanitiser. To comply with the minimum requirement for masks for all patients we will provide masks at a small extra cost which will be added to the consultation fee. Ensure that your patient cleans their hands-on arrival and on departure. They will be required to wear their surgical mask throughout their appointment. If the patient is unable to tolerate this instruction for any reason (try to encourage them to comply) you may terminate the session. Further information regarding the patient journey can be found elsewhere in this document. All masks should be disposed of with any other clinical waste.
- Appropriate PPE should be worn during every consultation and throughout patient contact. Further information regarding PPE can be found below, along with details of donning, doffing and disposal.
- Current advice is that all patient handling requires gloves, so they must be worn throughout the patient encounter.
- Ensure that paper towels and tissues are available to you and the patient throughout each appointment to allow for cleaning/personal hygiene.
- We will be allowing 15 minutes minimum between patients to allow for cleaning and aeration of the treatment room.
Personal Protective Equipment (PPE)
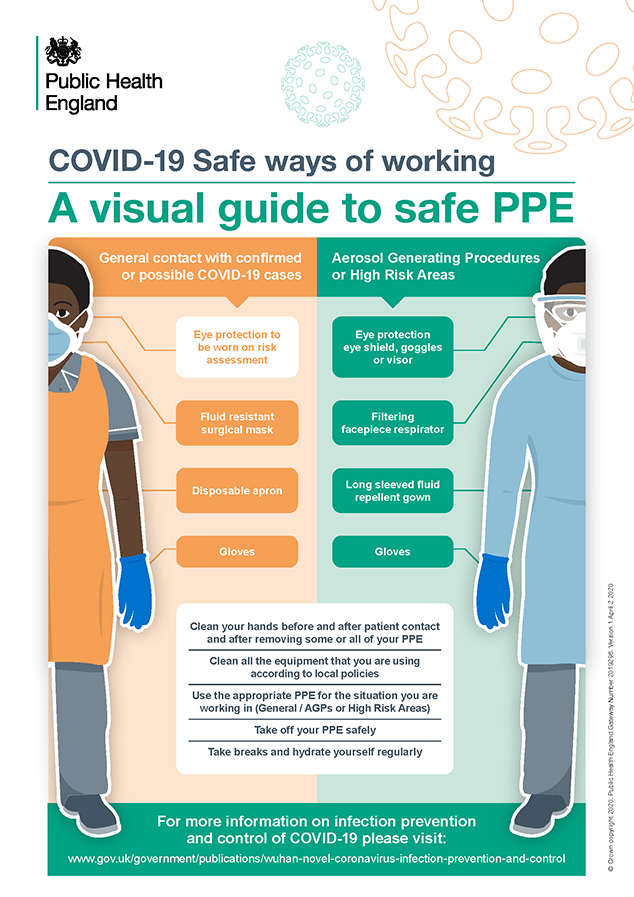
Guidance published by PHE[8] and summarised by NCOR[9] defines requirements for PPE as follows:
For direct patient care assessing an individual that is not currently a possible or confirmed case (within 2 metre zone) recommendations are to wear:
- Disposable gloves
- Disposable plastic apron
- Fluid resistant face mask (this can be a fluid resistant surgical mask, (FRSM Type IIR or better)). Further clarification from the iO distilled from the latest PHE guidance indicates that this type of mask “provides the level of protection required in most osteopathic contexts.”[10]
- We do not need to wear gloves whilst taking the patients case history. Gloves must be donned before any hands on contact with the patient.
The iO provides further clarification as follows:
Gloves
“Wearing gloves is a sensible precaution to reduce infection. An additional benefit of wearing gloves is that it changes behaviour. It is suggested that you are less likely to touch your face and contaminate yourself if you are wearing gloves. However, we appreciate that this is a significant change and may be challenging for some osteopaths.
Hand and forearm washing with soap and water is an essential part of infection control, whether these facilities are available in your clinic room or nearby. An appropriate sanitiser (60% alcohol or above) can also be used. Be mindful to take measures to protect your skin as the use of these products and/or repeated hand washing can cause dermatitis, which creates an increased risk of transmission of pathogens through broken skin. If you have signs of dermatitis or broken skin, then gloves should be used.”10
Also, “You should be bare below the elbow and it is recommended that hand hygiene should also be practised before putting on of gloves, including the washing of exposed forearms”10
Eye protection
Eye protection need only be worn “on a risk assessment basis where there is a risk of spray of blood or body fluids to the eyes, nose or mouth. Your decision to wear eye protection will be determined by your personal circumstances and acceptable risk levels. 10”In our clinical setting, eye protection would be appropriate if performing thoracic manipulation supine or where any technique may bring the face close to your patients and/or when a degree of chest compression may occur (eg sternal release techniques, deep breathing exercises).
Face masks
The maximum time you can use a facemask for would be a single session. A single session refers to a period of time where an osteopath is undertaking duties in a specific care setting/exposure environment. In NHS terms, one session is usually considered a half-day or up to 4 hours or when the clinician leaves the care setting/exposure environment. (PHE source)
They should be replaced sooner if:
- Dirty or
contaminated
- The PHE guidance also states that where clinician consider there is a risk to themselves or the individuals they are caring for, both osteopath and patient should wear a fluid repellent surgical mask (with or without eye protection dependant on the risk of droplet dispersion to the eyes), as determined by the individual staff member for the episode of care or single session. If there are none available the appointment should not continue and should be rescheduled if appropriate, or the patient should be referred elsewhere.
- Damaged
- Damp
- It is difficult to breathe through or uncomfortable
If performing an aerosol generating procedure (AGP) on a patient that is not a possible or confirmed case of COVID 19 recommendations are to wear:
- Disposable gloves
- A fluid repellent gown
- Filtering face piece respirator mask (such as FRSM type IIIR masks)
- Eye/face protection
There is no clarification yet as to whether any osteopathic techniques are considered AGPs (in medical practice they relate to procedures such as intubation, chest compressions etc) . Therefore, we are not proposing to use fluid repellent gowns or filtering respirator masks as a standard.
The following info-graphic summarises requirements.
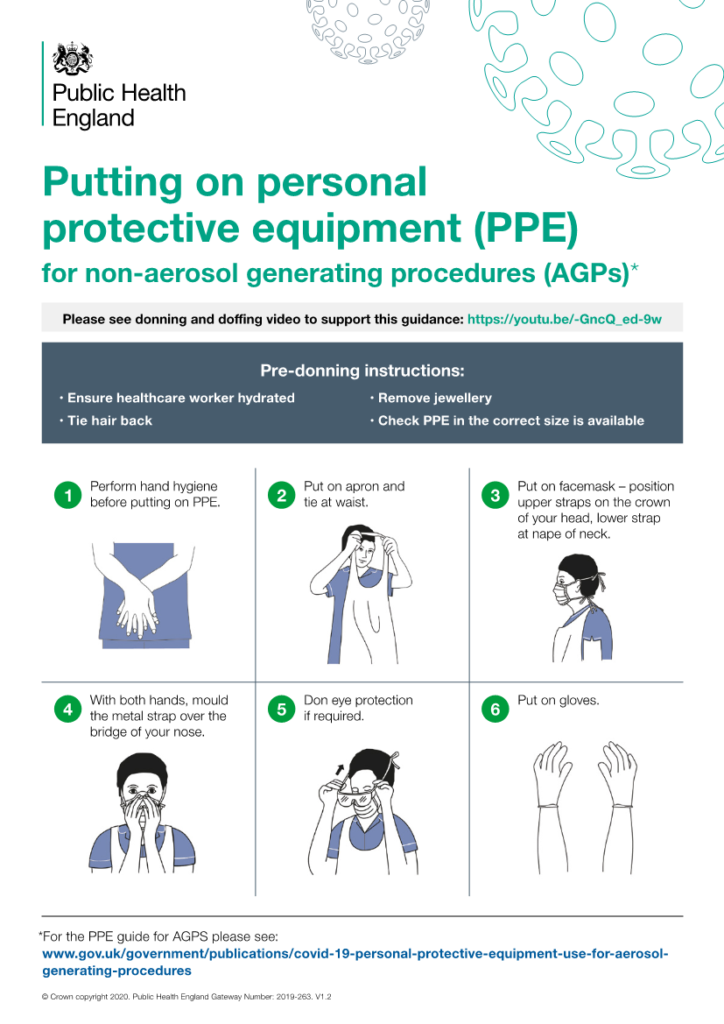
Putting on and taking off PPE
The order in which you put on (donning) or remove (doffing) your personal protective equipment is essential for protecting yourself and preventing the spread of any possible contaminants or fluids.
The following is the correct sequence for donning your PPE:
- Gown or apron;
- Mask or respirator;
- Goggles or face shields (If needed);
- Gloves.
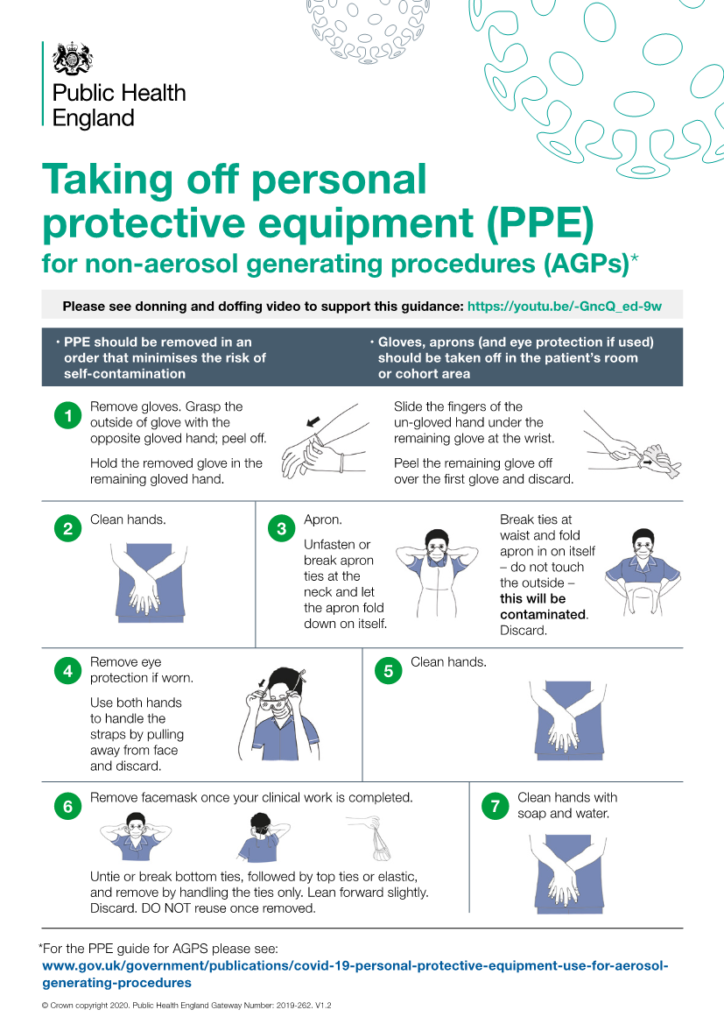
It is extremely important to take great care when removing and disposing of used PPE to avoid exposure to infection. It is important to practice before using these techniques in a clinical setting, ideally with a colleague to provide guidance and feedback.
The following is the correct sequence for doffing your PPE:
- Gloves;
- Face shield or goggles;
- Gown;
- Mask or respirator.
- Hand hygiene.
The sequence for removing PPE is intended to limit
opportunities for self-contamination. The gloves are considered the most
contaminated pieces of PPE and are therefore removed first.
Safe management of linen (laundry)
No special procedures are required; linen is categorised as ‘used’ or ‘infectious’. All linen used in the direct care of patients with suspected and confirmed COVID-19 should be managed as ‘infectious’ linen. Linen must be handled, transported and processed in a manner that prevents exposure to the skin and mucous membranes of staff, contamination of their clothing and the environment:
Disposable gloves and an apron should be worn when handling infectious linen.
All linen should be handled inside the treatment room. A laundry receptacle should be available as close as possible to the point of use for immediate linen deposit.
( are we still using paper roll on the couches )
When handling linen do not:
- Rinse, shake or sort linen on removal from beds/trolleys;
- Place used/infectious linen on the floor or any other surfaces e.g. a locker/table top;
- Re-handle used/infectious linen once bagged;
- Overfill laundry receptacles; or
- Place inappropriate items in the laundry receptacle e.g. used equipment/needles.
When managing infectious linen:
- Place directly into a water-soluble/alginate bag and secure;
- Place the water-soluble bag inside a clear polythene bag and secure;
- Place the polythene bag into the appropriately coloured (as per local policy) linen bag (hamper).
Store all used/infectious linen in a designated, safe, lockable area whilst awaiting uplift.
Staff uniforms/clothes
You will need to bring your work clothes with you separately. On arrival at the clinic you should change into your work attire and store your other clothes in the sealable box in the room if at the Royal Arsenal or in the box in the kitchen if at the Slade. The appropriate use of PPE will protect staff clothing from contamination in most circumstances.
Work clothes should be transported home in a disposable plastic bag. This bag should be disposed of into the household waste stream.
Work clothes should be laundered:
- Separately from other household linen;
- In a load not more than half the machine capacity;
- At the maximum temperature the fabric can tolerate, then ironed or tumbled-dried.
NB. It is best practice to change into and out of uniforms at work and not wear them when travelling; this is based on public perception rather than evidence of an infection risk.
Management of clinical and non-clinical waste
Disposal of all waste related to possible or
confirmed cases should be classified as infectious clinical waste suitable for
alternative treatment. It is suggested that all clinical waste should be double
bagged before being stored for a minimum of 3 days. This can then be disposed
of in the normal domestic waste. Therefore, if the bin bag requires emptying in
or at the end of your session time, double bag it, date it and leave it in the
kitchen if at the Slade or in the far right corner if at the Royal Arsenal. Do
not take it outside in the usual place behind Concierge if at the Royal
Arsenal. It can be take to the usual point after three days. If there is a
double bag in the corner which can go out, please take it to the back of
concierge so there isn’t a build up.
The typical patient journey
The following is a description of a typical patient journey and outlines a series of steps that should be taken to ensure appropriate measures are taken to minimise the risk of transmission of COVID-19 (A patient friendly version is included at the end of this document):
- Patients will only be allowed to book remote sessions online or by phone. Screening should be undertaken by an osteopath/ massage therapist prior to attending to establish whether the patient meets the initial criteria for an appointment and an initial assessment to identify if they are appropriate for osteopathic treatment.
- If a face -to-face appointment is not indicated the patient should be offered appropriate advice and or exercise prescription. They should also be advised about other care options too. Refer to another health professional if appropriate.
- Patients should be provided with standard advice on how to find the clinic (if they have not been before) and information about what they should expect when they attend for treatment. This will be further documented in the patients confirmation email. And will include detail as to why we are taking these precautions and how they are designed to protect people from infection. Additional information will be available on the website and through social medial. Ensure that the patient understands that we will be providing a new 3 ply fluid resistant mask and nitrate gloves to ensure the adequate protection for them, the therapist and for others using the room after them. There will be a £2.00 charge to cover costs which will be added to the session fee.
- Emphasis should be place on development of symptoms and to contact us if they become unwell. ALL reminders (48 hr email, 24 hr email and 2 hr text) all request for the patient to contact us if they feel unwell.
- Patients will be asked to turn up on time and to avoid arriving too early for their appointment. It might be best for them to wait in their cars until their appointment time if they arrive early. At the Royal Arsenal the osteopath will meet the patient outside reception with hand sanitiser and a mask. The patient should be offered use of the toilet prior to consultation to avoid the need for them to leave the treatment room during the appointment. Advice should be given to ensure 2 metre distance between any members of staff or public as appropriate. Royal Arsenal patients should be offered gloves in the room. At the Slade they can wait in reception after buzzing in where there is a prompt to use the sanitiser on the wall. The therapist will meet them in reception with a mask and gloves.
- During the initial triage you will need to perform a risk assessment to determine if the patient is symptomatic. Take the patients temperature using the gun. If deemed contagious, you will need to escort the patient off the premises and instruct them to return home and self-isolate for 7 days. Ventilate and clean the room and restrict access for at least 3 hours (preferably 48 hrs). If you have patients afterwards they will need to be contacted and rebooked.
- Following the consultation (or if the patient has been asked to leave), the decision as to whether the patient should be re-booked for a face-to-face or online appointment should be made in discussion with the patient and should take into account the risk of COVID-19 infection. Additional advice and guidance should be offered using Physiotec if appropriate. (The therapist should rebook the patient in room)
- If payment needs to be taken, it should be done at the end of the appointment via the secure Jane App. It should be explained to patients that their card details will be saved on our system unless they would like them removed immediately after payment. Wipe down any surfaces that the patient has touched and clean the floor with the mop provided.
The typical practitioner journey.
- It is important that the osteopath is mindful of their own health. They should take thie own temperature at the beginning of each session and record it as a ‘break’ on their diary and routinely assess their health status so that, should they begin to exhibit coronavirus symptoms, they should inform the clinic and self-isolate in accordance with current government guidelines.
- On arrival the osteopath should remove any outdoor clothing and store it in the sealable plastic container provided and don their work clothes. They should then disinfect their hands and clean the clinic wearing a disposable gown and gloves. All surfaces should be sprayed and wiped including door handles, computer keyboard and mouse, phone handset and other clinical and administrative equipment to be used.
- At the allotted time at the Royal Arsenal patients should be called to ensure they have arrived outside of the reception, don your mask before meeting them with hand sanitiser and mask. Remember, do not shake hands and maintain social distancing. They should be asked if they need to use the toilet prior to their appointment to limit the risk of cross infection outside the treatment room. Invite them into the clinic room, if they have used the toilet or touched door handles on their way in ask them to wash their hands before giving them gloves. At the Slade your patient should buzz at their appointment time and allowed in remotely. Meet them in reception and ensure that they have used the hand sanitiser provided on the wall before giving them gloves and mask. Invite them to use the toilet if necessary before taking them into the clinic room.
- Once in the room take and record their temperature and you should explain to the patient what they should expect during the session and the steps we are taking to protect them and ourselves from infection.
- Initial triage should re-evaluate whether or not the patient has coronavirus symptoms.
- If deemed contagious the appointment should be drawn to a close. Explain to the patient why the appointment cannot continue, escort the patient off the premises and instruct them to return home and self-isolate for 7 days. Ventilate and clean the room and restrict access for at least 3 hours (preferably 48 hrs). If locking the room is not possible an immediate clean is paramount. No fee will be charged.
- After your initial triage, if you still feel that it is appropriate to treat the patient, you should don your PPE and proceed as normal. You are not required to wear eye protection unless you feel that it is clinically necessary. For further clarification please read the section on PPE.
- Following the consultation (or if the patient has been asked to leave), the decision as to whether the patient should be re-booked for a face-to-face or online appointment should be made in discussion with the patient and should take into account the risk of COVID-19 infection. Additional advice and guidance should be offered using Physiotec.
- You should ensure that your case history documents precautions taken, the risks, benefits and treatment options available to the patient (including doing nothing) and note that you explained the risk of infection with the patient and that they were happy to go ahead with the appointment.
- Payment for the appointment should taken via Jane secure payment. Explain to the patient that their card details will be saved on the system unless they wish to remove them immediately after payment. Avoid taking cash.
- Once the patient has left the clinic the treatment room should be cleaned and aired as discussed in the cleaning and hygiene section.
- At the end of the morning and afternoon sessions you must perform a deep clean of the treatment room. All clinical waste and linen should be handled in accordance with advice elsewhere in this document.
What if a recent patient informs me that they have been diagnosed with COVID-19?
Recent guidance from the iO has provided further clarification around this point[11]
- If a patient who attended the clinic subsequently rings us to let us know that they have been diagnosed with coronavirus it is important that we take steps to trace all people who could have potentially been exposed to infection. (it is our responsibility to call all the patients seen subsequently that day ?)
- Use of PPE will lower the risk of transmission from you to other patients, but does not mitigate all risk, and therefore it is advised that you follow the guidance outlined here.
- The current evidence suggests the infectious period may begin before symptoms appear, with a consensus that is around 2.5 days, with the most infectious phase being around the day of onset. People are likely most infectious during the symptomatic period, even if symptoms are mild or non-specific.
- The iO are recommending that if a patient experiences symptoms within 2 to 3 days of visiting the clinic, any clinician with direct contact to that individual should self-isolate as per government guidance and then follow the return to work advice.
- Anyone with indirect contact with the patient during their visit, e.g. other patients in the clinic at that time, or staff not in direct contact, should be advised of the situation and suggest they monitor for symptoms. The advice from 111 is that people with indirect contact will not need to self-isolate.
- As a courtesy, you may wish to inform patients that you have seen in the 2 to 3 day period since seeing the symptomatic patient – regardless of small or high risk – as the vulnerability of the patient and their close relatives may be an important factor for the patient to consider.
- They should be advised to monitor themselves for symptoms and should be advised to self-isolate for 7 days if they become symptomatic.
Appendix 1: The patient journey
During the current pandemic we have introduced a number of measures to protect everyone from the risk of infection with COVID-19 whilst also being able to treat you effectively. We have taken steps to modify our clinics to enable us to maintain the recommended hygiene standards, introduced pre-appointment assessments to identify how best to care for you at present and introduced personal protective equipment (PPE) for staff and for you to wear to minimise the risk of spreading the virus. This means that your experience as a patient will be very different to what you are familiar with. To help you better understand what to expect the following guide describes how we will be working for the time being. Please take time to read it so you know what to expect. If you have any questions or concerns do not hesitate to contact us.
- At present you will only be able to book remote consultations either by phone or online with a view of a face to face if appropriate and at the discretion of the therapist. This will involve us asking questions about your current health (to ensure you do not vulnerable or have any symptoms of coronavirus) and the problem you need help with. We may decide that it is not be advisable to see you face to face.
- If a face-to-face appointment is not appropriate at this time we are able to offer advice or referral. We have been using this service during lock down and it has proved to be very effective in helping patients reduce their symptoms. We will also advise you about other care options too.
- If you are having an appointment with us we will require that you pay via our secure practice software. The system automatically saves your card details which we can delete immediately if you do not want us to save until your next visit. At this stage we do not intend to handle any cash. If you are unable to pay online or by card please let us know.
- New guidelines for face to face appointments require that patients wear a mask and gloves. To ensure required standards we will be providing appropriate masks at a £2.00 cost which will be added to your fee.
- Before you attend, we will tell you how to find the clinic (if you have not been before) and information about what to expect when you attend for treatment. This will also be described in your confirmation email. We will explain about the precautions we are taking and how they are designed to protect you from infection. Additional information is available on the website and through social media.
- We ask you to arrive as close to your appointment time as possible to avoid contact with others. When having appointments at the Royal Arsenal there is a two person limit in reception at concierge. You should arrive in enough time to pick up your parking permit and find a parking space. It may be best to wait in your car until your nearer your appointment time. Since we have no influence with infection control in the concierge reception we are asking for you to wait outside at your appointment time when your therapist will come out to meet you. If you arrive wearing your own gloves you will be asked to remove them as this is not good practice. Your therapist will have sanitiser and a masks for you. Please use the toilets if you need to before going into the clinic room so we can avoid the need for you to leave the room during your appointment. You will be asked to wash your hands again if you have used the toilet or door handles and given gloves to wear.
- When you arrive at the Slade you should buzz to be allowed into the reception where you can wait for your appointment. There is hand sanitiser for your use on the wall. Your therapist will meet you with gloves and mask. Please use the toilet before your appointment and if you need to. All our appointments will be staggered to avoid patients ‘crossing over’ and again reducing any potential risk of infection.
- Whilst in the room we will take and record your temperature.
- We will ensure that we maintain a safe distance whilst we take your details and case history.
- Your therapist will also put on protective clothing, including a disposable apron, face mask and gloves. This is to ensure that we are taking best care of you to reduce the risk of possibly spreading the virus.
- If, during the initial stage of your appointment you describe symptoms of coronavirus infection we will not be able to treat you. If this is the case you will not be charged for your appointment . We will escort you from the building and will you need to return home and self-isolate for 7 days. If you have any further concerns, you can ring NHS 111 to discuss your situation.
- Following the consultation (or if the patient has been asked to leave), the decision as to whether to book you another appointment will be made in discussion with your osteopath and will take into account the risk of COVID-19 infection. We can also offer you additional advice and guidance to help you manage your symptoms at home.
Appendix 2: Booking an appointment
Guidance for speaking to patients over the phone: Receptionists:
You are not expected to make any diagnostic decisions when booking a patient appointment.
Before we book you an appointment can we ask some questions
- “Because of the current situation we need to check that anyone coming to the clinic is safe to do so and therefore only taking remote sessions initially to screen and to take as much information as possible to reduce contact time. Any face to face appointments are at the discretion of the therapist and if not decided to be appropriate may be on an advice basis only and/or referral to a more appropriate health professional’
Please explain that the remote session work best with Chrome or Firefox and on either a desk or laptop, may take up to 30 minutes and should be organised for a private location as personal questions may be asked. It may be useful to be able to move freely in front of the screen if the therapist requires to see a movement or body part.
The appointment confirmation email will a link for them to follow
and contain an intake form for them to complete and have further information
about what to expect during their appointment. Please ask them to read through
this before they attend if they have not been to the clinic during the
pandemic.
[1] https://www.osteopathy.org.uk/standards/guidance-for-osteopaths/coronavirus-covid-19/
[2] https://www.iosteopathy.org/covid-19/clinical-guidance/
[3] https://www.ncor.org.uk/news/considerations-for-infection-prevention-and-control-and-personal-protective-equipment-for-osteopaths/
[4] https://www.gov.uk/government/collections/coronavirus-covid-19-list-of-guidance
[5] https://www.iosteopathy.org/covid-19/clinical-guidance/
[6] https://www.osteopathy.org.uk/news-and-resources/document-library/about-the-gosc/statement-on-remote-consultations/
[7] https://www.iosteopathy.org/wp-content/uploads/2020/03/iO-guide-to-conducting-tele-video-consultations.pdf
[8]https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/881489/COVID-19_Infection_prevention_and_control_guidance_complete.pdf
[9] https://www.ncor.org.uk/wp-content/uploads/2020/05/Considerations-for-Infection-prevention-and-control-and-personal-protective-equipment-in-osteopathic-practice-3.pdf
[10] https://www.iosteopathy.org/wp-content/uploads/2020/05/iO-infection-control-and-PPE-in-osteopathic-practice-052020-V1.pdf
[11] https://www.iosteopathy.org/covid-19/faq/

